With new cases of coronavirus (COVID-19) still being reported every day across the globe, we are starkly reminded that handling or coming into close contact with wildlife, their body parts, and excreta poses a risk of spillover of the pathogens [viruses, bacteria, parasites, and fungi] they host and maintain in nature, and to which we humans might be susceptible.
The illnesses animals spread to humans are known as zoonotic diseases, or zoonoses.
It is estimated that, globally, about one billion cases of human illness and millions of deaths occur every year from zoonoses. Some 60 percent of emerging infectious diseases that are reported globally are zoonoses and of the more than 30 new human pathogens detected in the last three decades, 75 percent have originated in animals.
A wide variety of vertebrates are carriers of zoonotic agents. Rodents, the most abundant mammal, also represent an abundant source of zoonotic diseases, carrying at least 180 unique zoonotic pathogens[1]. Because of their size, the ability to fly and their unique immune system, bats represent an important virus reservoir, though presently they are known to carry only about a third of the zoonotic pathogens that rodents do.
While there are fewer species of primates when compared to rodents and bats, a great proportion are zoonotic hosts. The risk that pathogens can infect humans increases with species more closely related to us. For example, the spillover of HIV to humans occurred from chimpanzees and sooty mangabeys, most likely through butchering and consumption of their meat. To date, HIV-AIDS has infected 75 million people and caused 32 million deaths[2].
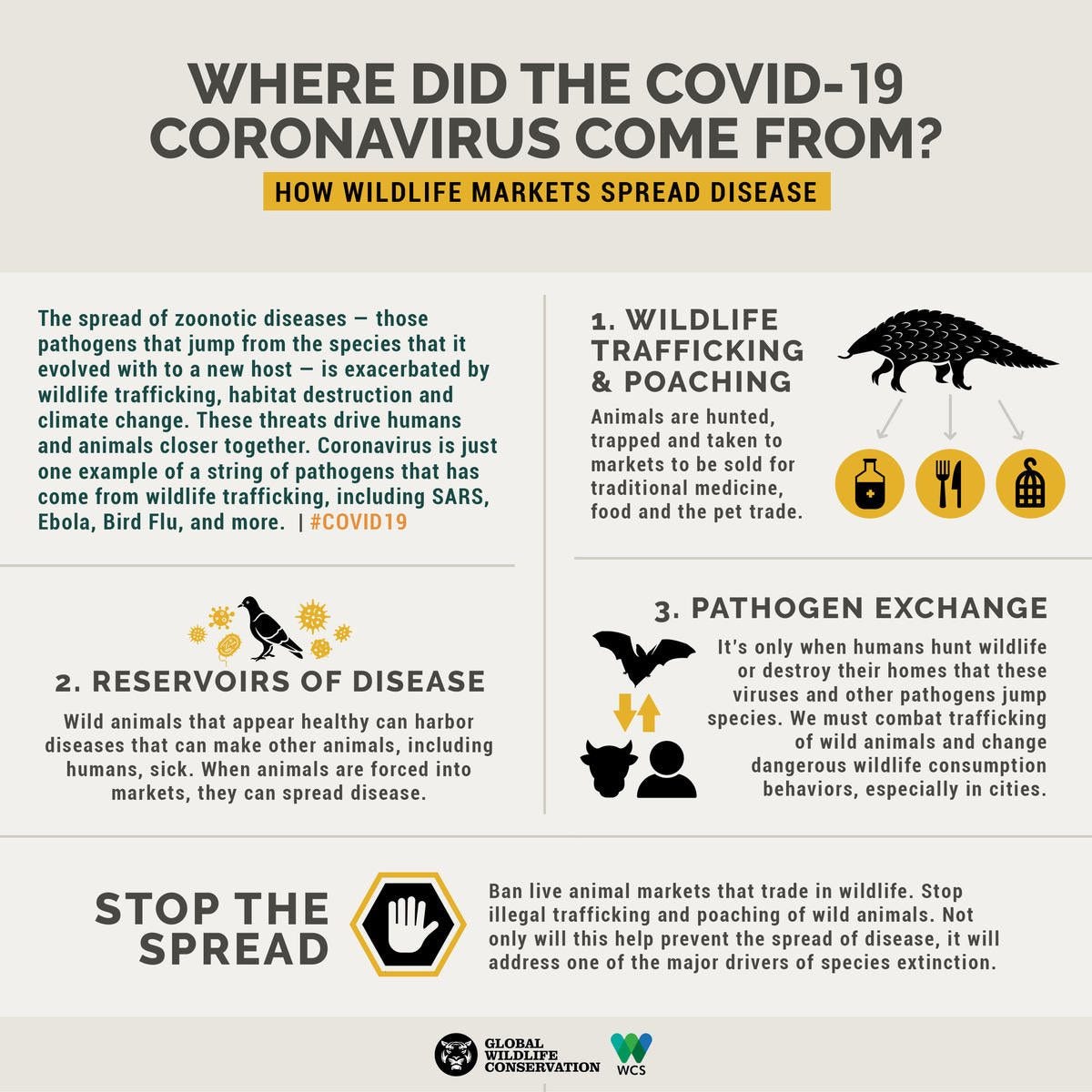 Graphic design: Sarah Markes/WCS.
Graphic design: Sarah Markes/WCS.
The persistent lethal capacity of zoonotic pathogens can also reside in its evolutionary strategies. Plague is a bacterial, vector-born disease transmitted by fleas from rodents –its natural reservoir– to humans and subsequently also from humans to humans that has impacted the history of mankind through multiple pandemics causing tens of millions of deaths worldwide. The responsible bacterial agent has evolved virulence factors that have allowed it to repeatedly and successfully evade the immune system of the mammalian host[3].
“Coming into close contact with wildlife — including their body parts and excreta — poses a risk of spillover of the pathogens they host, to which we humans might be susceptible.”
Zoonoses may exist in various forms: The most common, endemic zoonoses, are widespread in developing countries affect many people and animals and are by comparison mostly neglected by the international community, epidemic zoonoses vary widely in their duration and distribution and emerging and re-emerging zoonoses may or may not have occurred previously in a given population, but are generally observed to expand in new species, populations or areas.
Emerging infectious diseases (EIDs) and particularly zoonotic ones are a significant and growing threat to global health, global economy and global security. Analyses of their trends suggest that their frequency and economic impact are on the rise.
 The conditions of so-called “wet markets” are ideal for incubating new diseases and bolster their transmission. Photo credit: Elizabeth L. Bennett/WCS
The conditions of so-called “wet markets” are ideal for incubating new diseases and bolster their transmission. Photo credit: Elizabeth L. Bennett/WCS
Recent examples of such emerging or re-emerging zoonoses include Rift Valley fever, severe acute respiratory syndrome (SARS), pandemic influenza, Yellow fever, Avian Influenza, West Nile virus, the Middle East respiratory syndrome coronavirus (MERS), and most recently COVID-19.
However, our current knowledge of zoonotic diseases and spillover mechanisms is still at its infancy. It is estimated that less than 0.1% of all viruses that may pose a threat to global health are now known to have been transmitted from animals to humans[4].
More than 300,000 viruses are estimated to await discovery in mammals, many of them bearing zoonotic potential. In the U.S.-funded PREDICT program, researchers estimate that there are more than 1.6 million unknown viral species in mammals and birds, 700,000 of which could pose a disease risk to humans, based on years of information gathering.
“In wet markets across the globe, live and dead animals — including many wildlife species — are sold for human consumption.”
Facing such a vast, unknown and unpredictable universe of zoonotic agents, we firmly believe that limiting the chances of contact between human and wild animals is the most effective way to reduce the risk of emergence of new zoonotic diseases.
In “wet markets” across the globe, live and dead animals — including many wildlife species — are sold for human consumption. In close quarters, a mix of saliva, blood, urine and other bodily fluids brush up against vendors and consumers alike. The conditions of these markets are ideal for incubating new diseases and bolster their transmission. They form one of the most detrimental bridges created by man over the natural barriers that previously separated humans and wild animals.

Destruction of nature is increasingly putting humans in contact with pathogens for which they have no natural immunity. Photo credit: Nick Hawkins
For example, in 2016, two officials from the Department of Livestock and Fisheries in Lao PDR, Drs. Bounlom Douangngeun and Watthana Theppangna along with One Health experts authored a paper which documented that wild mammals from 12 taxonomic families and capable of hosting 36 different known zoonotic pathogens were traded in only seven markets[5]. It is a similar situation that has enabled the emergence of the previously unknown SARS in central Guangdong Province in November 2002 and now COVID-19 coronavirus in Wuhan, China.
“Ignoring the danger posed by wildlife markets is a massive global public health liability for a healthy world.”
The interface within these wet markets has been largely ignored as a public health topic, but COVID-19 coronavirus has brought this interface back to the forefront and reminded us that ignoring the danger posed by wildlife markets is a massive global public health liability for a healthy world.
As Dr. Christian Walzer emphasized recently this is a “global health priority that cannot be ignored.” It is important to continue calling for three solutions to prevent this complex global challenge: close live animal markets that sell wildlife; strengthen efforts to combat trafficking of wild animals within countries and across borders; and work to change dangerous wildlife consumption behaviors, especially in cities.
For the Silo, Stephen Sautner- Executive Director of Communications, Wildlife Conservation Society- Bronx Zoo
NOTES
[1] Cleaveland et al. 2001. Diseases of humans and their domestic mammals: pathogen characteristics, host rage and the risk of emergence. Phil Trans R Soc Lond B 356, 991–999
[2] Huet T, Cheynier R, Meyerhans A. et al. « Genetic organization of a chimpanzee lentivirus related to HIV-1 » Nature 1990, 345;356–9.
Santiago ML, Range F, Keele BF, Li Y, Bailes E, Bibollet-Ruche F, Fruteau C, Noë R, Peeters M, Brookfield JF, Shaw GM, Sharp PM, Hahn BH (2005). “Simian Immunodeficiency Virus Infection in Free-Ranging Sooty Mangabeys (Cercocebus atys atys) from the Tai Forest, Cote d’Ivoire: Implications for the Origin of Epidemic Human Immunodeficiency Virus Type 2”. Journal of Virology. 79 (19): 12515–27.
https://www.unaids.org/en/resources/fact-sheet
[3] Demeure C.E., Dussurget O., Mas Fiol G., Le Guern A.-S., Savin C., & Pizarro-Cerda, J. 2019. Yersinia pestis and plague : an updated view on evolution, virulenvce determinants, immune subversion, vaccination and diagnostics. Genes & Immunity 20, 357–370.
[4] http://livescience.ecohealthalliance.org/predict/reports/2018-04-16-edi-measuring-viral-discovery.pdf
[5] Zoe F Greatorex & Sarah H Olson & Sinpakone Singhalath & Soubanh Silithammavong & Kongsy Khammavong & Amanda E Fine & Wendy Weisman & Bounlom Douangngeun & Watthana Theppangna & Lucy Keatts & Martin G, 2016. “Wildlife Trade and Human Health in Lao PDR: An Assessment of the Zoonotic Disease Risk in Markets,” PLOS ONE, Public Library of Science, vol. 11(3), pages 1–17, March.


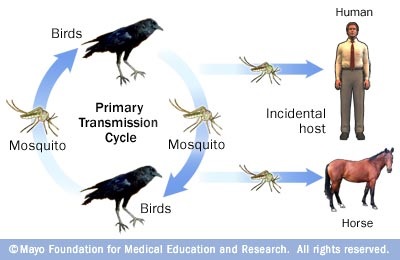
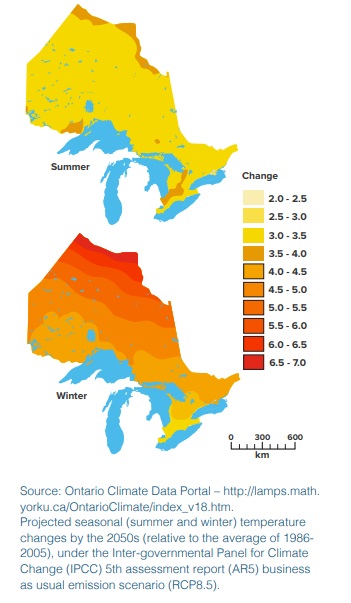 Milder winters and hotter summers create a paradise for insect and plant diseases. Are you getting more tick and mosquito bites? Lyme disease and West Nile virus, and other mosquito and tick-borne diseases, have been moving northward as our part of the world warms. And with increasing temperatures and phosphorus loads, many have taken notice of
Milder winters and hotter summers create a paradise for insect and plant diseases. Are you getting more tick and mosquito bites? Lyme disease and West Nile virus, and other mosquito and tick-borne diseases, have been moving northward as our part of the world warms. And with increasing temperatures and phosphorus loads, many have taken notice of